The Mindfulness Response: Homelessness, Mania, PTSD, Depression, Advocacy
- amindfulnessrespon
- May 1, 2024
- 9 min read
Notes from outpatient mental health group therapy
Mania and Homelessness
A manic episode can cause extra energy. Participants told others that they walked for hours, drove, went running, or were exercising endlessly, or were involved in reading an 800-page book in a few days. When manic, participants said other family members told them what they did, and some did not recall what happened.
Some manic behaviors can be reckless and cause trouble. One participant said they went off all medications and just wanted to be free and independent because there were no mental health problems. Another said they hitchhiked alone to other cities in nearby states and were homeless. Then, my family got involved and became my guardian.
Another member had paranoia and talked openly about street drug use and how he got several thousands of miles away from his home, when manic. When the family found him, the participant was underweight and unkempt from being homeless. The participant talked about working at a fast food restaurant but left the job when manic and admitted that times were tough on the street.
PTSD (Post-Traumatic Stress Disorder)
Being homeless allows a participant to move from one place to the next, whenever they feel triggered by past distress. Nightmares, flashbacks, and irritability related to avoiding people can cause a person to run from places associated with past trauma are a main part of PTSD.
PTSD symptoms can come and go at different times in people’s lives. Being homeless is dangerous. A person moves from one place to the next without any certainty of shelter, food, or sanitation. Trauma from combat or past abuse can negatively affect a person’s ability to manage stress daily. When PTSD symptoms arise, irritability, poor concentration, and being hyper-vigilant can be overwhelming for people. It takes a lot of energy to be constantly on guard and watching everything in the environment, just to avoid a trigger for a flashback. Nightmares can be debilitating.
A participant said they were afraid to be alone at night because of the nightmares. Other group members agreed that nightmares made it difficult to get back to sleep. Another participant said they did better when they stayed at a friend’s house and were not alone.
Sometimes flashbacks are visual memories, but participants talked about flashbacks being sounds, touches, smells, tastes, or other sensations. One participant talked about nightmares of trauma and realized that being on inpatient mental health was a trauma issue for me because they couldn’t control what their mind wanted to do since the body was doing something else.
Another participant talked about past trauma issues from an abusive relationship feeling guilty and ashamed for staying in the relationship. The participant said that flashbacks caused dissociation and panic attacks and didn’t always feel as if they were physically in their body.
Abuse:
There are many types of abuse. Participants discussed relationship problems with verbal, emotional, physical, or sexual abuse. One participant told others about taking advantage of personal finances when a person is disabled and may not understand all financial transactions.
Verbal/emotional abuse: name-calling, blaming, scapegoats, swearing, sexual harassment
Physical abuse: pushing, shoving, hitting, pinching, punching
Sexual abuse: unwanted sexual touch of any nature
Substance Abuse
Participants talked about past problems with street drugs, and alcohol that interfere with family, school, work, and relationships. Being unable to cut down, having arguments and others annoyed by your behaviors, and getting drunk or high with constant abuse of a substance were problems. After continued use, those abusing substances need an eye opener in the morning to get out of bed. (CAGE-AID).
Depression and Suicide Attempts
Discussions in group therapy focus on the desperation felt when a participant is in a dark, deep pit and can’t see any light. Other group members validate their feelings and tell them how grateful they are for that participant being in the group. Suicide attempts are painful memories and the group acknowledged that it is not the true participant's heart that wants to die, but the severity of the symptoms that takes over and creates the dangerous situation. It is not something they intended to do, but something to end their emotional pain. Another participant talked about the voices commanding orders to do something and how they criticized and swore daily at the participant.
Sexual Orientation Issues
Participants can have difficulty with sexual orientation. One participant admitted to not knowing how to identify and have relationships with all genders. Participants talk about the trouble with conservative families or relatives who don’t accept that they are not heterosexual.
Parents and children who differ in opinions about religion, politics, discipline, family issues, etc. Lengthy discussions in group therapy centered around childhood messages from family or religious leaders who had opinions that didn’t match their sexual orientation. How to live with differences requires acknowledgment, acceptance, patience, and flexibility. Not every participant felt supported by family, and some left their religion.
Acceptance and Self-Compassion
Self-compassion has three interrelated concepts. They involve understanding different parts of yourself and how you relate or connect with others. It involves your inner dialogue with yourself and being able to understand your thoughts, feelings, actions, images, and sensations. Using it in everyday life will change your attitudes towards others and yourself.
Three Concepts of Self-Compassion:
Mindfulness
Common humanity
Self-kindness
To do mindfulness, you are asked to accept any thoughts, feelings, images, or sensations that come into your mind. Acceptance of oneself as well as acceptance of others, for who they are and where they are in life is observed.
A participant talked of how they got stuck in old habits, got trapped by their bad habits, and had difficulty breaking their old patterns of behavior. One participant talked about addiction and being homeless. The participant got help to break the cycle of addiction, poverty, and despair.
A supportive person needs to be able to remain non-judgmental and listen to their story to help bring about change. Without this change process, the ability to reach and help a person who is homeless get therapy, psychiatry, medical care, and a safe, stable place to live is futile. Mental health treatment is not amazingly effective with homeless participants.
Although the physiological needs and safety needs are emphasized, it appears that those higher on the hierarchy model are less likely to be achieved. It leads a person with disabilities to believe that they may never be able to achieve aesthetic needs or self-actualization. All the levels are equally important, and this is further described with concepts of self-compassion.
Through conversations with group therapy members, it is evident that people have interactions between levels, and that the relationships on different levels can affect each other. At different times in our lives, we may be focused on different levels, and the hierarchy doesn’t match what life presents. The conversations from group therapy addressed all levels of the triangle in ways that were not hierarchical.
Gain Insight and Apply Skills
The participants talked about accepting how their situation was unmanageable and needed help to change it. Agreeing to work with a supportive person and develop a team of providers was one step in the right direction. A participant talked about how they got help to remain sober and found housing. Agreeing to work together as a team takes collaboration, and willingness to be open about symptoms and needs.
Patience
Patience creates understanding about the situation and trying to understand how it came about helps develop a team relationship. Group discussions centered around self-kindness and applying patience to the healing process.
Listen
Allow each team member to explain their ideas. Listening can be more important than talking. Gathering information from all team members about resources. Putting ideas to use and making plans takes time to organize and try new treatments, medications, or living situations.
Empathize
Participants told others they were grateful that support people could meet them where they were. The group discussed being able to listen and accept what they are doing and not feel devalued. The participants said they were challenged to stay sober and give up their lives on the streets and agreed to accept help.
Understanding
Participants talked about shame and guilt in their situation. They told others that they were trying the best that they could, under the circumstances. Participants talked about daily survival to find food, stay clean, wear clean clothes, and find shelter. Some talked about begging, prostitution, or stealing. Participants told other group members about how they burned bridges and were estranged from family and friends.
Be Non-Judgmental
Participants talked about feeling so low that they were suicidal. They recalled others criticizing, labeling them, or swearing or insulting them. They talked about how it created more hopelessness, depression, and anxiety.
Acceptance
The participants discussed how they survived on the streets. They made decisions in their lives that created many unexpected problems. One participant talked about the family's rejection of their values. The decisions, for good or bad, affect the participant today. Some participants became entrapped by their circumstances and did not know how to stop the cycle.
Trust
The participant talked about not trusting the family and that there were trust issues on both sides of the table. The participant did not want to show up when the family requested and did not trust their actions or their word. The group discussed how trust is built over time. Trust may not come immediately.
One participant talked about moving into a new residence and not being on any medication. The participant noted that the process was a struggle, and it became a crisis when they became psychotic. The family member and other team members kept communication open to establish a safer lifestyle. With a safe place to talk openly, the participant felt heard by family and providers and was prescribed medications to help reduce psychotic symptoms.
Offer Opportunities and Alternatives
It’s hard to be homeless during cold, rainy, snowy, or hot weather. There may be few alternative shelters for bad weather, or when they are ill. A conversation about shelter from severe weather was a motivator for one participant.
Reality Checks
One participant told the group how family helped do reality checks. Problems with misperceptions were cleared up and worries were resolved after considering thoughts and feelings about customers or co-workers.
Become an Advocate
Participants talked about resources and how their team helped them with paperwork to get stable housing or medical care, psychiatry, and psychology. Participants talked about their team of providers, being homeless, and how they were later able to become stable and return to work, college, or their community. One talked about becoming a mentor to youth who were at-risk and how it reminded them of their problems as a younger person.
Transformation / Making Changes: A Team Approach to Recovery and Healing
Participants shared their resources with others about collaborating with a team of professionals in the community. Participants were encouraged to get regular physicals to see their primary care physician (PCP) and be open with other specialty healthcare providers. One participant noticed that the voices were louder and criticized more after feeling ill for over a week. The participant was able to talk to their clinic about symptoms and get help to treat viruses, flu, or other illnesses that get out of control.
Participants started individual therapy after talking to the group about past regrets or trauma. The group pointed out that it can affect their ability to motivate themselves and continue with a daily routine. Medications are extremely helpful for managing severe symptoms. The program recommended a consultation with a psychiatrist for participants with severe symptoms.
Ensuring a safe home environment is vital. Some participants worked with housing managers or case managers to obtain stable housing. Once they had stable housing, they focused on longer-term goals that were interrupted by their mental illness.
Building a Supportive Team
Have a supportive person who listens and is frank and non-judgmental with you.
Have a psychiatrist who can help manage physical health and mental health issues.
Do
Stay sober.
Stay on prescribed medications.
Open and honest communication: medication side effects or other problems
Equipment; computer, monitor, Wi-Fi, and internet connections, for online therapy
Transportation to appointments
Stable physical health, and regular check-ups with PCP.
Safe and stable housing
Adequate food and a healthy diet
Keep appointments, make appointments with health care professionals.
A Supportive Person is Necessary
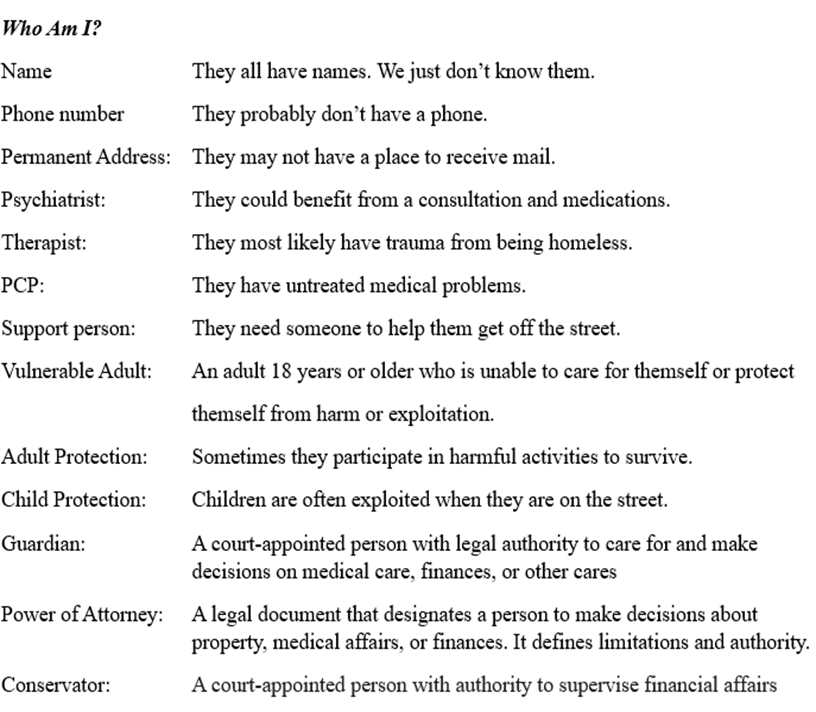
A supportive person is someone who can be non-judgmental and give frank responses to high levels of anxiety, paranoia, voices, or other psychosis symptoms. The supportive person can help with reality checks so that the individual can continue with their daily routine and learn to disregard the psychosis symptoms. The support person can advocate for a variety of treatment options or can help the individual advocate for themselves and be assertive with providers. Sometimes there are case managers from the county or region that can help with treatment, or legal systems are needed to establish guardianship, conservatorship, POA, Rep-payees, legal holds to be admitted for inpatient mental health treatment, or entry into outpatient treatment. To stabilize symptoms, a supportive person can help bridge the gap between the severe symptoms and treatment.
Supportive person
Name _________________________________________________________
Address _______________________________________________________
Phone ______________________ Email ______________________________



Comments